Anaphylaxis Management
Anaphylaxis Management
What’s Anaphylaxis
Anaphylaxis is a severe, rapidly progressive allergic reaction that is potentially life-threatening. Although allergic reactions are common in children, severe life-threatening allergic reactions are uncommon and deaths are rare. However, deaths have occurred and anaphylaxis must therefore be regarded as a medical emergency requiring a rapid response.
What are the main causes?
Research shows that students in the 10-18 year age group are at greatest risk of suffering a fatal anaphylactic reaction. Certain foods and insect stings are the most common causes of anaphylaxis. Eight foods cause ninety-five percent of food allergic reactions in Australia and can be common causes of anaphylaxis:
- peanuts;
- tree nuts (i.e. hazelnuts, cashews, almonds, walnuts, pistachios, macadamias, Brazil nuts, pecans, chestnuts, and pine nuts);
- eggs;
- cow’s milk;
- wheat;
- soy;
- fish and shellfish (e.g. oysters, lobsters, clams, mussels, shrimps, crabs, and prawns); and
- sesame seeds.
Other common allergens include some insect stings, particularly bee stings but also wasp and jumper jack ant stings, tick bites, some medications (e.g. antibiotics and anesthetic drugs), and latex.
Signs and Symptoms
Mild to moderate allergic reactions can include:
- swelling of the lips, face, and eyes;
- hives or welts;
- tingling mouth; and
- abdominal pain and/or vomiting (these are signs of a severe allergic reaction to insects).
Anaphylaxis (severe allergic reaction) can include:
- Difficult/noisy breathing
- Swelling of tongue
- Swelling/tightness in the throat
- Difficulty talking and/or hoarse voice
- Wheeze or persistent cough
- Persistent dizziness or collapse
- Pale and floppy (young children)
- Vomiting and/or abdominal pain for insect stings/bites
Symptoms usually develop within 10 minutes to several hours after exposure to an allergen but can appear within a few minutes.
Treatment of Anaphylaxis
Adrenaline given as an injection into the muscle of the outer mid-thigh is the most effective first-aid treatment for an Anaphylactic Reaction. Children diagnosed as being at risk of anaphylaxis are prescribed Adrenaline Autoinjectors in an emergency. The two most common brands of Adrenaline Autoinjectors available in Australia are EpiPen® and Anapen®300. Children between 10 and 20 kilograms are prescribed a smaller dosage of adrenaline in the form of EpiPen®Jr or Anapen®150. A child greater than 20 kilograms is prescribed an Adult EpiPen. These Adrenaline Autoinjectors are designed so that anyone can use them in the case of an emergency.
Sirius College recommends following the procedure below in the event that an Anaphylactic Reaction occurs.
Immediate Action
Remove the allergen
(Example. Nutella Sandwich)
Call for help
- Send 2 nominated students to the office with the child’s Emergency Card
- Students will return to the location with a staff member and the Child’s EpiPen
- Use the classroom phone or personal phone to notify the office or to call an ambulance
- Send another student to the buddy classroom to notify the teacher for assistance
- The teacher will remove other students from the classroom if deemed necessary
- The teacher will ensure students’ safety in the yard/outside of the classroom setting as assessed at the time.
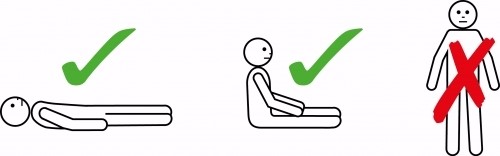
Lay the Student Flat or in a Sitting Position if the student has difficulty breathing
- Do NOT allow the student to walk, this is very dangerous
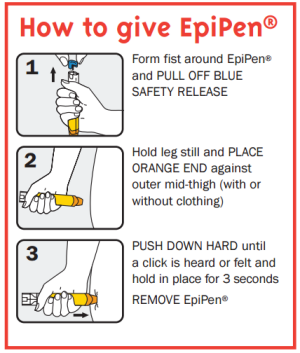
Administer EpiPen
| How to administer an EpiPen® | |
| 1. | Remove from the plastic container. |
| 2. | Form a fist around EpiPen® and pull off the blue safety cap. |
| 3. | Place the orange end against the student’s outer mid-thigh (with or without clothing). |
| 4. | Push down hard until a click is heard or felt and hold in place for 3 seconds. |
| 5. | Remove EpiPen®. |
| 8. | Note the time you administered the EpiPen®. A second injection may be needed if there is a delay in the ambulance’s arrival or if the first injection is not effective. Emergency services will inform you if this is needed. |
| 9. | The used auto-injector must be handed to the ambulance paramedics along with the time of administration. |
| How to administer an AnaPen® | |
| 1. | Remove from the box container and check the expiry date. |
| 2. | Remove the black needle shield. |
| 3. | Form a fist around Anapen® and remember to have your thumb in reach of the red button, then remove the grey safety cap. |
| 4. | Place the needle end against the student’s outer mid-thigh. |
| 5. | Press the red button with your thumb so it clicks and hold it for 3 seconds. |
| 6. | Replace the needle shield and note the time you administered the Anapen®. |
| 7. | The used auto-injector must be handed to the ambulance paramedics along with the time of administration. |
Please ensure you take the time to update your anaphylaxis training online. Please click the link below on the correct use of an EpiPen.
Please click on the link below to watch a video on the correct use of an EpiPen.
In the event that an anaphylactic reaction occurs, an ambulance will be called to have the child assessed and taken to the hospital for further monitoring. The child’s nominated caregiver (Parent/Guardian) will be notified.
A follow-up with the students, families, and staff involved is recommended as this can be a traumatic experience. It is recommended that the College’s counselors conduct a debriefing session.
All students who are at risk of an anaphylactic reaction require an ASCIA Action Plan to be submitted annually and reviewed when there is any change in the child’s condition or if any reactions occur. Sirius College cannot exclude a student from school for not providing an action plan. It is acceptable however to exclude a child from attending camps or excursions. Students should also have an individual anaphylaxis management plan which is developed with the child’s parents.
Prevention strategies
Classroom Recommendations
- Liaise with parents about food-related activities ahead of time.
- Use non-food treats where possible. If food treats are necessary, it is recommended that parents of students with food allergies provide a treat box with suitable alternatives. These treat boxes should be clearly labeled and only handled by the respective student.
- Never give food from outside sources to a student who is at risk of anaphylaxis.
- Do not serve products labeled as ‘may contain traces of nuts’ to students with nut allergies, and similarly, do not serve products labeled as ‘may contain milk or egg’ to students with milk or egg allergies, and so on.
- Ensure all cooking utensils, preparation dishes, plates, knives, forks, etc. are washed and cleaned thoroughly after preparation of food and cooking.
- Have regular discussions with students about the importance of washing hands, eating their own food, and not sharing food.
Canteen Recommendations
- Canteen staff (whether internal or external) should be able to demonstrate satisfactory training in food allergen management and its implications on food-handling practices, including knowledge of the major food allergens triggering anaphylaxis, cross-contamination issues specific to food allergy, label reading, etc.
- Helpful resources for food services: http://www.allergyfacts.org.au/component/virtuemart/
- Canteen staff, including volunteers, should be briefed about students at risk of anaphylaxis,
- Display the list of students at risk of anaphylaxis with their names and photos as a reminder.
- Do not serve products labeled as ‘may contain traces of nuts’ to students with nut allergies, and similarly, do not serve products labeled as ‘may contain milk or egg’ to students with milk or egg allergies, and so on.
- Canteens should provide a range of healthy meals/products that exclude peanut or other nut products in the ingredient list or a ‘may contain…’ statement.
- Make sure that tables and surfaces are wiped down with warm soapy water regularly.
Yard Duty
- Carry emergency cards in yard-duty bags and mobile phones,
- Be aware of the Emergency Response Procedures and how to notify the general office/first aid team of an anaphylactic reaction in the yard,
- Be able to identify, by face, those students at risk of anaphylaxis,
- Keep lawns and clover mowed and outdoor bins covered.
- Students should keep drinks and food covered while outdoors.
Using Bus Service
- Ensure an Adrenaline Autoinjector available on the bus,
- Ensure either the student can self-administer or another person can administer an Adrenaline Autoinjector.
Excursions and Sporting Events
- Avoid using food in activities or games, including as rewards.
- Consult with Parents of anaphylactic students in advance to develop an alternative food menu, or parents provide a meal (if required)
Camps and remote settings
- Consult with the camp provider whether they can provide food that is safe for anaphylactic students.
- The camp cook must demonstrate satisfactory training in food allergen management, including an understanding of the major food allergens that can trigger anaphylaxis, knowledge of cross-contamination risks related to food allergies, and proficiency in reading food labels.
- Review the camp provider’s emergency response procedures to ensure they are adequate in the event of an anaphylactic reaction.
- Consider bringing an Adrenaline Autoinjector for General Use on a College camp, even if there are no students at risk of anaphylaxis, as a backup device in case of an emergency.
- Students with anaphylactic reactions to insects should always wear closed shoes and long-sleeved garments when outdoors, and they should be encouraged to avoid areas with water or flowering plants.
- Cooking, arts, and crafts activities should not include the use of known allergens.
- Be mindful of potential allergen exposure when consuming food on buses and in cabins.
Overseas travel
- Plan for appropriate supervision of students at risk of anaphylaxis at all times,
- Record details of travel insurance, including contact details for the insurer.
- Determine how any costs associated with medication, treatment and/or alteration to the travel plans as a result of an anaphylactic reaction can be paid.
- Evaluate the Emergency Response Procedures and, if needed, modify them to suit the specific conditions of the overseas trip.